Why patients and Stakeholders Demand Better Digital Health Information Sharing
If you live in Texas and go on a vacation to a remote part of Mongolia with your credit cards in hand, you will be able to survive as far as there is an ATM close by and stores that accept major credit cards.
This financial data connectivity contrasts with our wacky healthcare information exchange in the US, whereby two hospitals or clinics across the street from each other in the same vicinity cannot successfully exchange health data.
This ability to seamlessly exchange health data between different systems, like electronic health record (EHR) vendors, insurance companies, clinics, etc., is called Interoperability [1]. There is almost no interoperability between the major EHR systems in the US.
To make matters worse, a recent study showed that Interoperability was also poor within the same organization using the same HER[1].
The waste in the form of undue duplication of tests and procedures, delays in treatment, and workflow burdens that result from lack of Interoperability are harmful to patients and hurt our collective public health.
The US government’s 21st-century Cures Act has banned information blocking to overcome this lack of health data interconnectivity. Hospitals, clinicians, and vendors must grant unhindered patient data access on demand[2,3].
The 21st Century Cures Act (the Cures Act) of 2016 was signed into law to improve the flow of electronic health information. The ultimate aim is to strengthen research, advance medical innovation and product development, and improve patient care[2,3].
The law prohibits health information blocking mandates interoperability, enhanced usability, accessibility, privacy, and security of health information technology[4].
The law only grants exceptions to information blocking in particular circumstances like privacy and security concerns, preventing patient harm, infeasibility of information sharing, etc[5]. See the graphics below.
Who are the highest culprits of information blocking in healthcare
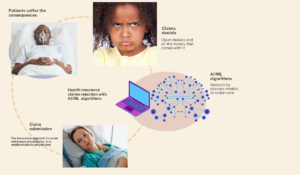
Unexpectedly, more clinicians block patients from their medical health information data than healthcare vendors[ 7]. Yikes!, I am sorry to tell you that my “tribe” of doctors are more guilty of this offense.
Out of the 250 information blocking complaints filed to the Office of the National Coordinator for Health IT (ONC), 77% of complaints were filed against clinicians, and just about 17% were filed against vendors[6,7].

Without fixing fundamental issues of interoperability and data silos, there is no way we can reap the benefit of big data and AI in healthcare
Ahmed-digital doc Tweet
Digital health 360 degrees lens
What are some of the issues causing information-blocking among clinicians?
A law without straightforward ways of enforcement is pretty much dead on arrival. Although the government has set standards for data sharing, the Office of the National Coordination (ONC) only recently announced a fine of $1 million against any organization that commits information blocking[8]
Additionally, the government still lacks an “end-to-end process from complaint to enforcement action with feedback loops. They have yet to announce the manner of enforcement.
The fact that clinicians and doctors are the most significant culprits warrants further analysis.
Could it be because of the government’s lack of clear enforcement guidelines?
Another possibility is the lack of knowledge on how to go about the technology infrastructure and workflow required to implement the anti-blocking policy.
Another often overlooked problem with Interoperability is the lack of standardization and variations in how different health systems implement their EHR software.
For example, an oncologist’s essential information to determine treatment modality is a receptor status called HER2 receptor in breast cancer treatment.
This crucial “life or death” information is not easily exchanged between the same EHR record for a patient because it is not standardized when transcribed from a pathologist’s report[1].
Undoubtedly, the US EHR implementation was in a hurry, and Interoperability was not a priority ab initio. However, it’s time to rise above the hype of the “digital revolution” in health care.
Without fixing fundamental issues like interoperability and data silos, there is no way we can reap the benefit of big data and AI in healthcare.
References
- Interoperability sucks even within the same EHR; https://academic.oup.com/jamia/article/29/5/753/6500181
2. FDA 21st century cures act; https://www.fda.gov/regulatory-information/selected-amendments-fdc-act/21st-century-cures- act#:~:text=The%2021st%20Century%20Cures%20Act,them%20faster%20and%20more%20efficiently.
- 21st century cures act NIH; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424829/
- Information blocking def; https://www.facs.org/advocacy/regulatory-issues/advocacy-quality/new-information-blocking-rules/
- Exceptions to information blocking; https://www.healthit.gov/topic/information-blocking
- Information blocking claims; https://www.healthit.gov/data/quickstats/information-blocking-claims-numbers
7.Information blocking claims, STAT; https://www.statnews.com/2022/03/10/health-information-blocking-complaints/
- 1million information blocking fine; https://www.statnews.com/2023/09/05/health-tech-information-blocking/