Breast cancer disproportionately impacts women of color. Black women are more likely to die from breast cancer at every age. The incidence of breast cancer is higher in black women and other women of color compared to non-Hispanic whites[1].
The disparity is grounded in many socio-economic and environmental factors/social determinants of health (SDOH). SDOH includes a lack of adequate access to preventive health/screening.
Due to these factors, women of color undergo screening mammograms far less than non-Hispanic white women[2].
The US Preventive Services Task Force (USPSTF) updated its screening mammogram guidelines for breast cancer (breast CA) in 2016. The USPTF is a government-funded panel of independent experts that develop recommendations for clinical preventive services[3].
Also, the Food and Drug Administration (FDA) recently approved Artificial intelligence-powered algorithms (AI) for breast CA screening and diagnosis[4, 5].
A combination of the updated guidelines and questionable methodology behind the approval of the breast CA algorithms is worsening breast CA disparity.
This article will analyze how both events aid breast CA disparity and objective ways of reducing breast CA disparity by stakeholders involved.
Is Breast cancer screening recommendation amplifying Breast cancer disparity?
In 2016, the USPSTF increased the recommended age for breast CA screening from forty to fifty, stating that screening at that age is more useful [6].
They reason that the risk of the false-positive test (overdiagnosis) was high before fifty years with a high incidence of unnecessary follow-up biosies[6].
This updated guideline, however, failed to account for ethnic differences in age-related breast cancer data for women of color and appears only to cater to the peak incidence in white women [6].
Black women are more likely to develop aggressive breast tumors earlier in life and at more advanced stages of the disease[5]. The incidence of breast CA before age 45 is higher among Black women, while breast CA incidence rate peaks above 60 years of age in non-Hispanic white women[5,7].
Algorithmic Bias as the Jet Fuel that Propels Breast Cancer Disparity
AI algorithm applications are becoming ubiquitous in healthcare. The FDA recently granted clearances to AI products for breast CA screening with the hope of better detection.
According to STAT investigations [4,5], only one of the ten breast cancer imaging algorithms cleared by the FDA breaks down the demographics of the data used to build the algorithm. Others hide behind “proprietary” information not to disclose[4].
The approval is flawed because the FDA does not mandate a public disclosure of whether their AI tools have was tested on people of color before approval.
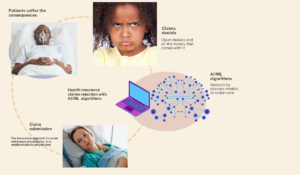
They are also not mandated to share the demographical composition of the data they are using to build the algorithm. The inability to verify this information increases disparity against women of color judging by recent similar events with algorithmic bias[8].
We already have erroneous, overhyped traditional algorithms and computer-aided detection (CAD) software for breast cancer that didn’t improve outcomes.
Mainly because there was no consideration for diverse racial demographics in their development, the Tyrer-Cuzick model overestimated the risk of breast CA in Hispanic patients[9].
The Gail model is another one that underestimated the risk of breast cancer in Black patients and overestimated the risk in Asian patients[10].
Vendors need to put more effort into obtaining real-world representative data for training algorithms beyond just scrapping training data from the internet, which has been proven times without number to be harmful
Ahmed-digital doc
Tweet
Digital health 360 degrees lens
Contrary to the USPSTF recommendation, many other expert institutions, like the National Consortium of Breast Centers and the American Society of Breast Surgeons, recommend breast CA screening at 40 years[6].
Nevertheless, USPTF recommendations are held in higher esteem by their pedigree and the backing of the US government. As such, USPSTF recommendations are usually the yardstick for payer reimbursement for screening procedures. This implies that health insurance will not cover a mammogram for a woman under 50.
The USPSTF recommendations have far-reaching implications for the healthcare of minority populations. As such, we recommend that social determinants of health be integral to decisions leading to a final screening recommendation.
Algorithmic bias is an unfortunate reality in our contemporary world. As a background to this global problem with AI health tools, just 7 of 161 healthcare AI products cleared in recent years by the FDA include any information about their datasets’ racial composition[5].
Although regulation is the cornerstone for preventing algorithmic harm, the heavy lifting needed to overcome this cannot come from regulators alone.
Vendors and AI institutions need to put more effort into obtaining real-world representative data for training algorithms beyond just scrapping training data from the internet, which has been proven times without number to be harmful.
Another good start to unraveling the unconscious bias in the data set is to hire a diverse team, at least include someone who lives the reality of the algorithms you are developing as part of your team. Checking a politically correct box by hiring a diversity officer is only the beginning.
Without undertaking these basic tasks, we would only be developing tools on “steroids” for a section of our society and amplifying systemic health injustice/racism.