Your physician is a time bomb waiting to explode, no kidding!
Just in case you were not aware, up to 60% of physicians in the U.S. experience burnout. Add on the fact that the suicide rate is highest amongst physicians compared to other professions [1,2,3]. Clinician burnout reduces the quality of care at the individual patient level and worsens overall public health outcomes.
Although we cannot accurately quantify the overall harm from burnout, its impact is increased physician turnover, which costs the U.S. healthcare sector about $4.6 billion/year[4].
In essence, this issue affects all of us, and we cannot afford to ignore it. No matter how you look at it, as a humanist or as a “dollar[ist]”
Navigating physician burnout and a deep dive into its causes
1. Changing overall healthcare landscape
Factors like an aging population, physician shortage, change from volume-based care to value-based care, and emerging patient as a customer model of medical practice are some drivers of clinician burnout. These rapid and concurrent changes adversely impact physicians and result in burnout [5]. Feel free to add more, including the Covid-19 pandemic.
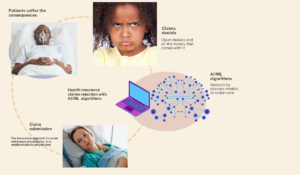
2. Increased Pressure from Regulators and Payers
Regulators and payers demand more accountability, improved healthcare quality, and a higher volume of patients per unit time at a reduced cost. These mandates put enormous pressure on clinicians and result in burnout.
Essentially, contemporary patients are sicker with more complex chronic medical problems now requiring more individualized physician attention, adding to the increasing elderly population as well as mental health crisis.
Despite all these, the regulators expect physicians to see more of these patients in less time without corresponding increased financial or time incentives. The consequence is physicians working overtime without compensation for the extra hours.
3. Technology induced; electronic health record (EHR) and its lack of usability
EHR implementation is associated with physician burnout[6]. The reasons include EHR usability/user-friendliness, demand for standardized documentation against free-flowing narrative texts, and redundant documentation.
Excessive data entry requirements, a lack of interoperability, and notes geared toward billing at the expense of actual patient care are the most common contributors to EHR-induced physician burnout [6].
Just as digital health and Medical informatics suffer from issues of “data silos”, there is also the problem of “Knowledge silos” as every institution keeps its knowledge siloed.
Although many institutions nationwide are involved in various unique projects to improve the EHR’s user-centeredness, there must be more protocols about specific ways to go about it or replicate their projects to enhance EHR in other institutions.
4. Overall change in the technological environment and consequence of the 4th industrial revolution
The 4th Industrial Revolution postulates how digital, physical, and biological technology have uniquely combined in our contemporary world, creating new opportunities and challenges.
This drive from legacy to digital systems demands that physicians adapt to changes quickly, which can be stressful and increase burnout. For more about 4th Industrial Revolution and healthcare, see this free ebook; https://www.intechopen.com/chapters/73581
The EHR ab-initio was conceptualized for efficient billing, not for patient care or research. It renders the machine a huge “cash register” and turns clinicians into cashiers.
Ahmed-Digital Doc Tweet
A user-centered-technology solution to reducing EHR-induced physician burnout
At Mount Sinai Hospital in NY, we piloted a project called Beyond Getting Rid of Stupid Stuff in the EHR (Beyond-GROSS), which expanded on Hawaii Pacific’s project Getting Rid of Stupid Stuff (GROSS)[7].
In Beyond-GROSS, we seek direct input from clinicians about redundant and frustrating aspects of the EHR and request they suggest possible solutions. The Beyond-GROSS team (physicians and nurses informaticists) receives their requests.
The project was well received, and clinician-participants are very happy about improvements and tweaks to the EHR that arose from their direct input.
We then collected data on the project’s outcome and impact data, with preliminary results showing high satisfaction with the project, reducing EHR burnout.
Although many other institutions may be involved in various unique projects to improve the EHR’s user-centeredness, more protocols need to be developed about specific ways to do this or replicate their projects to enhance EHR in other institutions.
Just as digital health and Medical informatics suffer from issues with “data silos,” there is also the problem of “Knowledge silos” as every institution keeps its knowledge locked in. Our team’s extra effort to publish this protocol is an attempt to share and alleviate the issues of knowledge silo in the EHR improvement ecosystem

Digital health 360 degrees lens
The problem of physician burnout is multifactorial etiology, including systemic issues of change in the healthcare environment, change in our overall technology landscape, and physicians’ inability to adapt to these changes while trying to provide quality care.
The regulators/payers have the most significant potential to reduce physician burnout.
Setting realistic expectations and compensating clinicians based on the complexity of their patient panel and not just the volume of patients seen will be a good start.
This also has far-reaching implications for reducing health inequity, as many physicians will not see the need to abandon their practices in high-needs and high-risk areas, which always correspond to areas of low social and economic status and minority populations.
Our Electronic health record system (EHR) is a hotbed of redundancies and is not user-centered. Nevertheless, the EHR is just a messenger and only functions based on how we developed it. We are to blame for EHR-induced physician burnout.
The EHR ab initio was conceptualized for efficient billing rather than for patient care or research. It renders the machine a huge “cash register” and turns clinicians into cashiers.
As clinicians, we also have a role to play in reducing burnout. Unfortunately, the solution requires manifesting skill sets that many of us suck at; adaptability and flexibility. Physicians and clinical medicine are highly structured and impervious to change.
Most of our principles and practices are from the Socrates era. Nevertheless, as the genie has left the bottle, we are at an “adapt or perish” stage; these factors will only worsen.
Physicians must leverage the advantages of the technological revolution to reduce their burnout.
For example, by now, every clinic should have a telemedicine option embedded in their practice; otherwise, they will miss out on the advantages it brings to reducing burnout.
References
- Jones GM, Roe NA, Louden L, Tubbs CR. Factors associated with burnout among us hospital clinical pharmacy practitioners: results of a nationwide pilot survey. Hosp Pharm. Dec 2017;52(11):742-751
- Dutheil F, Aubert C, Pereira B, et al. Suicide among physicians and healthcare workers: A systematic review and meta-analysis. PLoS One. 2019;14(12):e0226361. Published 2019 Dec 12. doi:10.1371/journal.pone.0226361
- Rothenberger DA. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017;60(6):567-576
- Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 4 2019;170(11):784-790
- Ahmed Umar Otokiti (October 26th 2020). Digital Health and Healthcare Quality: A Primer on the Evolving 4th Industrial Revolution [Online First], IntechOpen, DOI: