Why do couples undergoing infertility treatment need pre-implantation genetic testing (PGT)
Polygenic risk score (PRS) is a type of genetic test/scoring system. Unfortunately, no evidence-based research validates the PRS method for pre-implantation genetic testing[1]. It is akin to using an appropriate test for the wrong reason. Other evidence-based pre-implantation genetic tests (PGT) are available.
Yet some clinics offer it to infertility patients as the next best thing since sliced bread!
PGTs are various tests carried out on embryos before implantation. Different types of PGTs are available for patients undergoing infertility treatment. These tests assist infertility patients in increasing the chances of fetal viability and reducing pregnancy loss.
Also, performing these PGTs can prevent the implanting of a fetus with a debilitating (genetic) disease. For example, some rare genetic disorders run in some families.
If such disorders are present in both couples’ families, they may benefit from the PGT test.
Another instance is previous pregnancy failures due to fetal genetic disorders, as most early pregnancy losses are due to the fetus having genetic problems.
What is polygenic risk score (PRS), and why is it a “Digital health snake oil” in infertility treatment?
Our genetic advancement with whole-genome sequencing shows that many inherited genetic disorders result from the cumulative effects of different genes (polygenic in etiology)[2].
This polygenic theory is in contrast to our previous knowledge of Mendelian genetics, where most genetic disorders are due to the expression of one gene (monogenic)
The PRS was then developed based on this updated knowledge. The PRS aggregates many minor effects of contributing genes across the human genome to assess an individual’s risk of a disease or disease-related trait. This risk assessment combines relevant information like personal and family history, clinical findings, and disease biomarkers to ascertain overall risk.
We continue to overrate the impact of genetics on disease outcomes at the expense of environmental factors and do not realize that an individual’s zip code is more critical than their gene code.
John Doe
Tweet
Digital health 360 degrees lens
Unfortunately, taking undue advantage of patients’ medical problems is too familiar in our society. The International Common Disease Alliance’s PRS Task Force, a multidisciplinary group comprising genetics, law, and ethics experts, warns against using PRS[3].
Such genetic scam festers because we continue to overrate the impact of genetics on disease outcomes at the expense of environmental factors. Therefore, your Zip code is more critical than your gene code in disease outcome determination[4].
Essentially, even if you inherit excellent genes but lack the right environmental and systemic factors, a.k.a social determinants of health, you are highly unlikely to achieve your full potential.
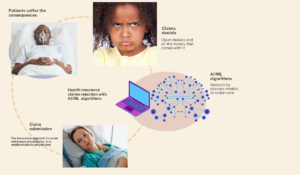
Implementing the wrong technology festers patient harm far beyond physical and mental injury. For example, Invitro fertilization is expensive, intrusive, and associated with risks. Even the standard evidence-based PGTs are not without risk.
Additionally, most infertility treatments have limited insurance payer coverage. Adding a test without utility to an already expensive process can increase infertility patients’ chances of bankruptcy.
Another sinister side to this test is the potential to become mainstream in the future despite no ethical basis for it[5].
In fact, according to a survey published in the journal Science, about 40% of U.S. adults said they would do such a test to choose embryos with a higher intelligence aptitude enough to complete a college degree in the future [6].
Should this trend continue, it will pour more gasoline on the fire of worsening societal disparity and inequality. Imagine a situation whereby only people of a particular socioeconomic status can afford to alter their embryos to produce more intelligent and healthier offspring[5].
This PRS has much potential in population and individual health to guide disease screening, prevent disease, and enhance personalized medicine therapy[3].
Using it for pre-implantation testing is a scam at this time. The solution to this problem lies in regulations mandating proper disclosure of pre-implantation testing to patients. The other solution is adequate patient education about PGT so that they can ask the right questions.
References
-
Polygenic risk score unethical use in pre-implantation testing; https://www.nature.com/articles/s41431-021-01000-x
Genome-wide polygenic risk score for disease identify disease like monogenic; https://pubmed.ncbi.nlm.nih.gov/30104762/
Responsible use of polygenic risk score in clinics; Polygenic Risk Score Task Force of the International Common Disease Alliance; https://pubmed.ncbi.nlm.nih.gov/34782789/
Forget genes: it’s your zip code that influences your health; https://www.weforum.org/agenda/2016/06/transforming-healthcare-for-the-low-income/
Americans are ready to test embryos for future college chances, survey shows;https://tinyurl.com/fhpw73wf
Public view of PGT https://www.science.org/doi/10.1126/science.ade1083